A new and simplified anion exchange chromatographic process for the purification of both live and inactivated cell-grown H1N1 influenza viruses was established with a recently developed anion exchanger. The resin is designed with an optimized surface extender and pore size for superior accessibility and large biomolecule binding capacity, aiming to overcome common drawbacks of existing ion exchangers for virus purification.
The H1N1 Influenza Virus
The influenza pandemic of 1918 killed 50 million people globally, and viral influenza still infects an estimated 3–5 million people annually, resulting in a quarter to half a million deaths per year.
There are two main types of influenza viruses — A and B — which can be further broken down into subtypes based on their surface proteins (Fig. 1). The hemagglutinin, or HA, protein and the neuraminidase, or NA, protein dictate the various subtypes. Regardless of type or subtype, all influenza viruses have the same basic structure: a spherical particle comprised of seven proteins.
The H1N1 influenza virus is a type A influenza virus also known as swine flu and was the strain behind the 1918 influenza pandemic. The most recent pandemic caused by the H1N1 influenza virus was the 2009 pandemic, although smaller outbreaks are common.
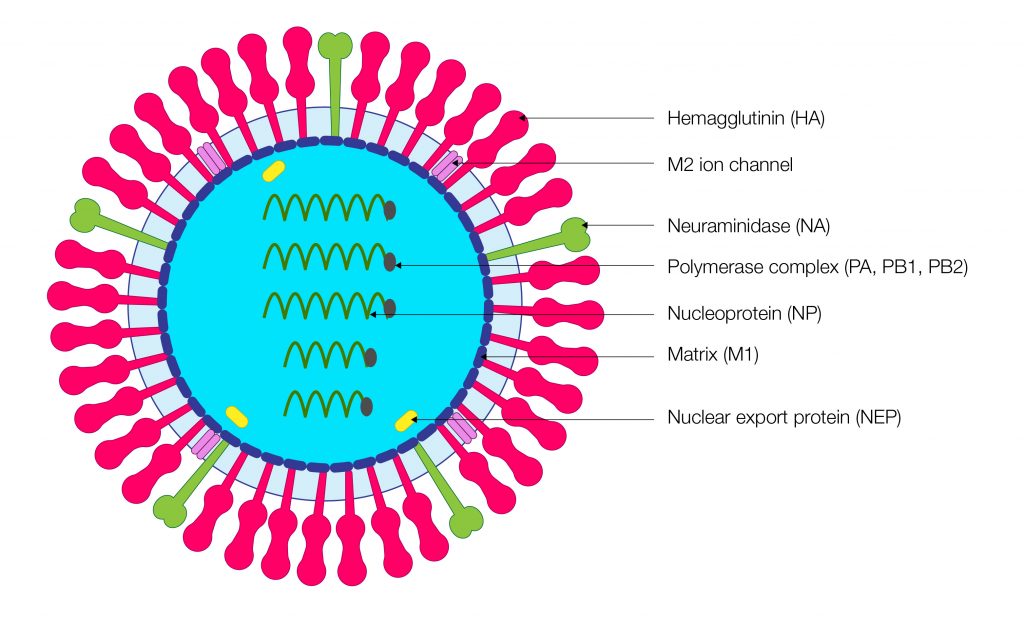
Figure 1. Schematic of influenza virus particle showing key surface proteins.
How Were Influenza (Flu) Vaccines Originally Made?
Manufacturing activated or live attenuated vaccines, such as the influenza vaccine, requires large quantities of virus. To obtain the amount of virus needed to make millions of doses of flu vaccines each year, manufacturers have traditionally used chicken eggs. Candidate vaccine viruses are injected into fertilized eggs and allowed to replicate (i.e., make many copies of the virus) for a few days. Viruses are then harvested from the eggs to make vaccines. Although this process has been used for over 70 years, it is time consuming, taking up to six months, and can be problematic for people with egg allergies. Recent technological advances in cell culture–based virus propagation have made vaccine production faster and more reliable.
Replicating Viruses in Animal Cells
The process of creating cell-based influenza vaccines involves several steps. First, the vaccine manufacturer inoculates the candidate vaccine virus into cultured mammalian cells (instead of into eggs) and allows it to replicate for a few days. Then, the virus-containing fluid is collected from the cells and the viral antigen is purified. The manufacturing process continues with further purification and testing. Finally, regulatory bodies (such as the U.S. Food and Drug Administration or the European Medicines Agency) test and approve the vaccines prior to release and shipment (U.S. Centers for Disease Control and Prevention).
Virus Purification Strategies
Virus purification is a critical step in cell-based vaccine production. Anion exchangers are an attractive option for virus purification because their cost-effectiveness, packing flexibility, and scalability can handle a sudden surge in vaccine demand caused by a pandemic (Duy et al. 2021). Several ongoing studies are investigating different chromatographic workflows, including ion-exchange, hydrophobic interaction, size exclusion, mixed-mode, and metal affinity.
Nuvia HP-Q Resin is a recently developed anion exchanger designed with an optimized surface extender and pore size for optimal accessibility as and binding capacity for large macromolecules such as plasma proteins, IgM, and IgA. This novel exchanger has not yet been explored for virus purification (Duy et al. 2021).
Our collaborators at Bioprocessing Technology Institute (BTI) Singapore therefore studied the performance of Nuvia HP-Q Resin for influenza virus purification, comparing it to other published methods (Duy et al. 2021). Nuvia HP-Q Resin, as a single capture purification step, resulted in high virus recovery and excellent impurity removal. Moreover, the workflow does not require nuclease treatment or intensive filtration of the H1N1 culture harvest prior to chromatography, which could significantly reduce overall purification costs.
Developing the Nuvia HP-Q Resin Workflow for Influenza Virus Purification
H1N1 viruses were injected into and propagated within the Vero cell line derived from Cercopithecus aethiops (African green monkey). Viruses were harvested after a 48-hour replication period and used in downstream experimental procedures to test the performance of the Nuvia HP-Q Resin for influenza virus purification. The purification workflow is summarized in Fig. 2.

Figure 2. Workflow for purification of H1N1 influenza virus particles with Nuvia HP-Q Resin. Figure courtesy of BTI Singapore.
To reduce large particles without effecting HA activity, microfiltration was the first step performed, resulting in 8.67 × 109 viral RNA copies/ml clarified supernatant. Next, several column studies using 1 ml Foresight Nuvia HP-Q Columns were performed to determine optimal binding conditions. These experiments revealed that the maximum volume of supernatant resulting in no detectable virus in the flowthrough of a 1 ml Foresight Nuvia Column was 199 ml (5.83 × 1011 viral RNA copies). The final operating conditions for influenza virus purification with Nuvia HP-Q Resin are summarized in Table 1.
Table 1. Optimized protocol for H1N1 influenza virus purification with Nuvia HP-Q Resin.
| Step | Mobile Phase | pH | CV | Remark |
| Equilibration | 20 mM Tris, 100 mM NaCI | 7.5 | 5 | |
| Sample loading | 20 mM Tris, 100 mM NaCI | 7.5 | – | 5.83 x 1011 viral RNA copies/ml of resin |
| Wash | 20 mM Tris, 100 mM NaCI | 7.5 | 10–30 | |
| Elution | 20 mM Tris, 590 mM NaCI | 7.5 | 10 | |
| High salt strip | 20 mM Tris, 1.5 M NaCI | 7.5 | 5 | |
| Clean in place | 1 M NaOH | >12 | 10 |
* Operational linear flow rate: 84 cm/hr.
The elution chromatogram for the optimized protocol shows that eluate with 590 nM NaCl contains high HA activity, indicating no significant aggregation of purified H1N1 virus (Fig. 3). H1N1 recovery and purity were also high, as seen in Table 2.
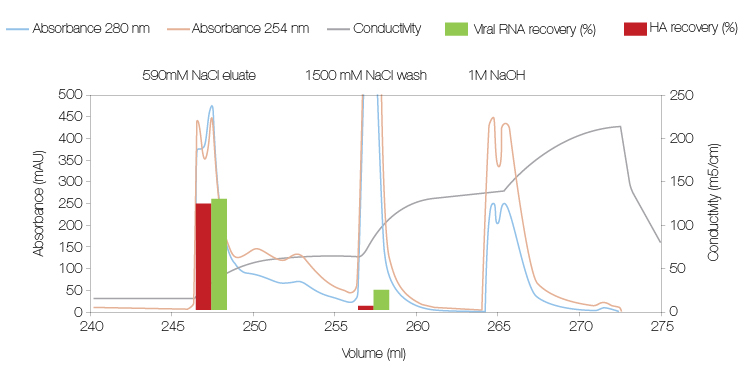
Figure 3. The elution chromatogram of clarified cell supernatant on the Nuvia HP-Q (1 ml column volume) using optimized protocol conditions. Figure courtesy of BTI Singapore.
Table 2. H1N1 virus recovery and purity using Nuvia HP-Q Resin for purification.
|
Purification Step |
HA Recovery, % |
Viral RNA recovery, % |
HCP/HA, mg/mg |
hcDNA/HA, ng/mg |
HCP removal, % |
hcDNA removal, % |
|
|
Culture supernatant |
100.0 |
100.0 |
13.9 |
442.5 |
– |
– |
|
|
Microfiltration |
100.0 |
169.5 |
13.0 |
221.3 |
6.5 |
40.8 |
|
|
Nuvia HP-Q Resin |
Moderate loading (7.51 × 1010 viral RNA copies/ml resin |
80.0 |
73.8 |
1.1 |
0.3 |
96.2 |
99.99 |
|
Maximal loading (5.83 × 1011 viral RNA copies/ml resin) |
70.7 |
73.7 |
2.1 |
0.0 |
95.0 |
100.0 |
|
HA, hemagglutinin; hcDNA, host cell DNA; HCP, host cell protein.
The recovery and purity obtained with Nuvia HP-Q Resin are excellent compared with the European Pharmacopoeia standards (European Medicines Agency, 2017) for a single vaccine dose (15 mg HA, ≤ 6.7 mg host cell protein (HCP)/mg HA, and ≤ 0.67 ng host cell DNA (hcDNA)/mg HA). Additionally, the result with Nuvia HP-Q Resin is excellent compared to other reported purification protocols, as summarized in Table 3.
Table 3. Summary of recovery and purity of reported purification protocols for the H1N1 virus.
|
Reported Purification Scheme |
HA Recovery, % |
HCP/HA, mg/mg |
hcDNA/HA, ng/mg |
HCP Removal, % |
hcDNA Removal, % |
Reference |
|
Filtration/Nuvia HP-Q Resin |
70.7 |
2.1 |
0.0 |
95.0 |
100.0 |
Workflow with Nuvia HP-Q Resin |
|
DF/MF/UF-SEC-AEC |
53.0 |
7.7 |
34.5 |
96.5 |
99.8 |
|
|
AEC-HIC |
92.2 |
17.2 |
2.0 |
58.4 |
99.0 |
|
|
AEC, monolith |
89.0 |
NA |
NA |
>52.0 |
>98.0 |
|
|
Pseudo-affinity, sulfated membrane |
94.2 |
2.1 |
23.0 |
57.1 |
68.1 |
|
|
Pseudo-affinity, sulfated membrane |
64.0 |
13 |
3.8 |
NA |
NA |
AEC, anion exchange chromatography; DF, diafiltration; HA, hemagglutinin; hcDNA, host cell DNA; HCP, host cell protein; HIC, hydrophobic interaction chromatography; MF, microfiltration; NA, not applicable; SEC, size exclusion chromatography; UF, ultrafiltration.
Concluding Remarks
Our results demonstrate that the Nuvia HP-Q resin has an excellent capacity for directly capturing H1N1 virus particles from cell culture supernatant clarified by microfiltration only. Under optimized conditions, 70–80% HA recovery was achieved with over 95% of host cell impurities removed in a single chromatographic step. Nuclease treatment, tangential flow filtration prior to chromatography, and a polishing step could be eliminated due to the capability of the HP-Q resin to efficiently separate HCP, nucleic acid contaminants, and virus aggregates from intact and active H1N1 virus particles. The results of this study suggest that a scalable, cost-effective downstream processing platform for influenza virus purification for vaccines is achievable.
For more information, please watch this presentation.
References
Carvalho SB et al. (2018). Purification of influenza virus-like particles using sulfated cellulose membrane adsorbers. J Chem Technol Biotechnol 93, 1988–1996.
Duy TT et al. (2021). A new and simplified anion exchange chromatographic process for the purification of cell-grown influenza A H1N1 virus. J Sep Pur Tech 263, 118412.
European Medicines Agency (2017). Guidelines on Influenza Vaccines — Quality Module. https://www.ema.europa.eu/en/documents/scientific-guideline/guideline-influenza-vaccines-quality-module-revision-1_en.pdf, accessed June 13, 2022.
Fischer LM et al. (2018). Purification of cell culture-derived influenza A virus via continuous anion exchange chromatography on monoliths. Vaccine 36, 3153–3160.
Kalbfus et al. (2007). Purification of cell culture‐derived human influenza A virus by size‐exclusion and anion‐exchange chromatography. Biotechnol Bioeng 96, 932–944.
Opitz L et al. (2009). Sulfated membrane adsorbers for economic pseudo-affinity capture of influenza virus particles. Biotechnol Bioeng 103, 1144–1154.
U.S. Centers for Disease Control and Prevention. How influenza (flu) vaccines are made. https://www.cdc.gov/flu/prevent/how-fluvaccine-made.htm, accessed June 13, 2022.
Wiegel et al. (2019). Hydrophobic-interaction chromatography for purification of influenza A and B virus. J Chromatogr B Analyt Technol Biomed Life Sci 1, 103–117.

